The Loss of Normal Birth in the UK
The New Normal.
Over the past two decades, the landscape of childbirth in the UK has changed beyond recognition. From campaigns promoting physiological birth to scandals, safety inquiries, and a growing midwifery crisis, the role of the birthkeeper is now more vital than ever.
This timeline maps the key events, reports, and policy shifts that have shaped the landscape of birth in the UK. Each moment marks a step away from physiological birth towards a system increasingly driven by fear, intervention, and risk management.
I was a midwife watching as the tide shifted, as older midwives retired and as the new midwives came in, and I knew the blanket induction policy at 41 weeks would seal the fate of birthing women and people. A fate that involved induction of labour, medicalised and traumatising births often ending in a caesarean that they did not expect or want.
This wasn’t about money. It was about a patriarchal medical model of pregnancy and birth that believes we are pieces of a machine to be fixed and saved.
Yet no one asked the women. Or the birthing people.
Timeline of Events
2005 – RCM Campaign for Normal Birth
Royal College of Midwives (RCM) launched the “Normal Birth” campaign to promote physiological birth and reduce unnecessary interventions.
2011–2015 – Morecambe Bay Inquiry
Investigation into serious maternity failings at Furness General Hospital (Morecambe Bay NHS Trust). Found 11 baby deaths and 1 maternal death (avoidable).
Impact: Major spotlight on safety; blamed pursuit of “normal birth at any cost”; led to loss of trust in “normal birth” campaigns.
2015 – Withdrawal of RCM’s Normal Birth Campaign
RCM quietly moved away from explicit “normal birth” language post-Morecambe Bay.
Reframed focus toward “Better Births for All”, prioritising safety and choice equally. Read more.
2016 – Better Births Report
A National Maternity Review led by Baroness Julia Cumberlege.
Key point: Strong push for Continuity of Carer — same midwife/team throughout pregnancy, birth, and postnatal.
Aim: Improve outcomes, reduce interventions, empower women and birthing people.
Impact: Patchy implementation, funding and staffing challenges. READ MORE HERE.
2016 onwards – Maternity Transformation Programme
7 national priorities including:
Safer care
Choice and personalisation
More midwife-led units
Continuity of carer
Impact: Ambitious, but slow and inconsistent rollout.
2016 – 2019 Saving Babies’ Lives Care Bundle
Aimed at reducing stillbirth and neonatal death.
Focused on smoking cessation, monitoring growth, reduced fetal movements, better monitoring during labour.
Impact: Some evidence of reduced stillbirths where fully implemented.
2019 – Ockenden Review (Interim report 2020, Final 2022)
Shrewsbury and Telford Hospital Trust.
Hundreds of avoidable deaths of babies and mothers.
Criticised a toxic culture, failures to investigate serious incidents, and pressure to achieve “normal birth” at all costs.
Impact: Tremendous damage to the trust in midwifery-led care models.
2019 onwards – Perineal Care Bundle
National initiative to reduce 3rd and 4th degree tears.
Encourages good communication, hand-placed support during crowning, warm compresses.
Impact: Also encourages episiotomy, semi recumbent position and lack of autonomy. READ MORE HERE.
2021 – MMBRACE Reports on Maternal Mortality
Repeated findings: Black women 3-4x more likely to die during pregnancy/childbirth. Asian women 2x more likely.
Impact: Increased public awareness; calls for systemic racism and inequality in maternity care to be addressed.
2021 – Birthrights Report on Homebirth/Birth Centre Closures
“Listening to Maternity Voices” report revealed widespread closure of standalone midwife-led units and suspended homebirth services (especially post-Covid).
Impact: Drastic reduction in access to physiological birth settings.
2023 – Birth Trauma Inquiry launched
First parliamentary inquiry into birth trauma, chaired by Theo Clarke MP and Rosie Duffield MP.
Gathering personal testimonies of trauma, highlighting systemic failings.
2024 – Proposal for National Induction at 41 Weeks
New recommendation to offer all pregnant women and birthing people induction by 41 weeks.
Impact: Raising concerns over autonomy, medicalisation of normal pregnancy, possible increase in interventions like caesarean sections.
2024 – Midwifery Crisis Escalates
Repeated RCM reports show critical shortage of 2,500+ midwives.
Mass burnout and resignation due to unsafe staffing levels.
Evidence: ONS workforce surveys; RCM “State of Maternity Services” reports; Health Foundation workforce analysis.
Where Are We Now?
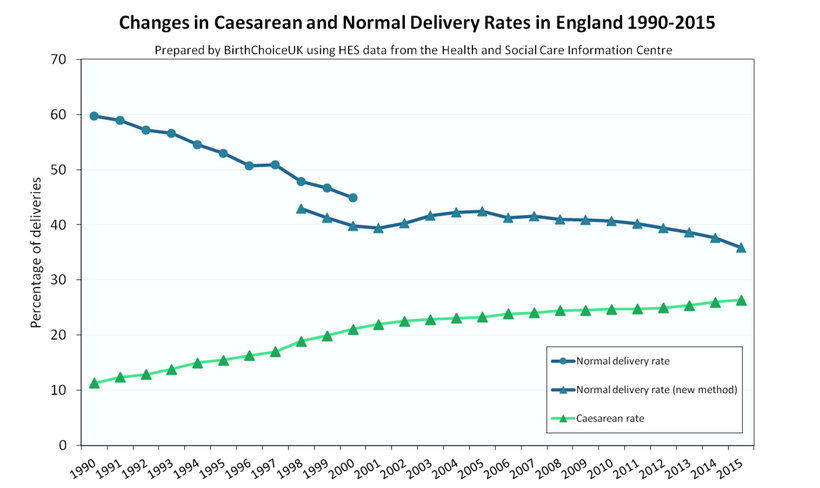
And the currents rates of caesarean are much higher, bordering on 50%. Induction around 40%. Normal vaginal births less than 50%.
We don’t yet know the impact of 41 week induction on stillbirth rates across the UK. The most recent MBRRACE-UK Perinatal Mortality Surveillance Report, covering babies born in 2022, was published on 11 July 2024 and gave a rate of 3.35 per 1,000 total births. But babies of Black ethnicity are still more than twice as likely to be stillborn than babies of White ethnicity (Black: 6.19 per 1,000 total births; White: 2.99 per 1,000 total births). The next report will be published in 2025 for babies born in 2023.
Why Birthkeepers and Doulas Must Be the Wise Ones Now
The crisis in maternity care hasn’t happened by accident: policies, political agendas, and institutional control have shaped a system where midwives are burnt out, isolated, and unable to practise the true art of midwifery. Researchers and advocates who raised concerns were often silenced or pushed out, and the medical model rooted in control and a patriarchal “saviour” mindset has replaced trust in physiological birth with fear and intervention. We now face a generation of midwives who, through no fault of their own, have rarely seen undisturbed birth and have lost the guidance of elders who once held that wisdom.
With the average career span of a midwife now around seven years (according to the WHELM study), it’s clear that no one inside the system is coming to save us. This is why intelligent, wise, and well-informed doulas and birthkeepers are needed more than ever — to bridge the gap, to understand the real landscape, and to offer a different way forward rooted in knowledge, compassion, and true support for women and birthing people.
If you’re thinking of training as a doula or birthkeeper check out my year long mentored programme: the Birth Doula Course.
Seriously, you are needed more than ever.